Pudendal neuralgia is significant malady that is more often than not misdiagnosed increasing the debility and the misery of those with this diagnosis. “
During my 15 years providing medical care in the field of Physical Medicine and Rehabilitation there has been no other outpatient pain syndrome that I have come across as debilitating and destructive to the life of a patient than the patients that I diagnosed as having pudendal neuralgia. I will discuss the symptoms by way presenting the ‘typical’ clinical history and the anatomic problem that causes the symptoms. The diagnostic tests required to make this diagnosis, and the treatments for this disorder are beyond the scope of this article but will be discussed by me in the future. Finally, I will discuss how the “vaginal mesh debacle” has brought this condition to the awareness of the medical community, and in a way will prevent the destruction of lives in the future by preventing the failure to diagnose and treat which essentially was the unfortunate standard of care that ‘modern medicine’ provided to these patients.
A Case Study:
Jan H., a 45 year old white female required a vaginal hysterectomy for abnormal uterine bleeding when she was 37 years old. Her post-operative course was complicated by a pelvic hematoma (bleeding) that required re-exploration to stop the pelvic bleeding. Post-operatively she had some right sided pelvic pain when she sat, which improved over a period of six week period to a slight ache. CT scan was ordered which showed resolution of her hematoma with no pelvic abnormalities. Her pain over a period of weeks changed in characteristic and worsened in terms of intensity. Her pain always intensified with prolonged sitting, especially on hard surfaces and with activities requiring bending and stooping activities. She was an avid gardener and had not been able to resume this activity since her surgery. She found comfort when reclining or while sitting on a toilet.
Over a three month period she began to have numbness down her right lower extremity to her foot, with buttock pain, which was worse sitting than standing. Her primary doctor ordered an MRI L-S which revealed an S1 disc herniation towards the right with slight impingement on the nerve root. She was sent to a neurosurgeon who performed a discectomy, which failed to improve her pain. Over a period of three months she began having some incontinence of urine, and occasionally had shooting pain to the right side of her anus which she described as a lancing pain. Her family doctor sent her to a urologist who ordered renal ultrasounds and an IVP to evaluate her for a kidney stone. She was told by the urologist that she was fine. Her family doctor then sent her to a gastroenterologist because of the anal pain and her complaints of constipation with a feeling that she could not evacuate her bowels. She underwent a colonoscopy and was told she had a hemorrhoid. Her family doctor sent her to a general surgeon who performed a hemorrhoidectomy. Her symptoms and pain continued and in fact worsened. She couldn’t sit for any extended period of time, any bending cause shooting pain to her buttock, and any activity worsened her pain. She was having right leg numbness with activity and ongoing incontinence and constipation. Repeat MRI of the lumbar spine could not identify any postoperative abnormality except some mild fibrosis (scar) on the nerve root. She was told by the neurosurgeon that she wasn’t a surgical candidate and that she would have to live with her pain and she was placed on disability.
She was then referred by her family physician to a pain management specialist who “gave her” the diagnosis of cauda equina syndrome. He prescribed narcotic pain medicines and an antidepressant. She underwent a series of epidural injections on the nerve root with some transient improvement. Her pain persisted despite these interventions and she underwent a dorsal column stimulator which helped to a small extent but she still required narcotics, antidepressants, and other medications to provide some relief of her pain. She required two hospitalizations of major depressive episodes and overdosed on her narcotics once as an attempt at suicide.
Currently, her complaints include shooting pain to her right buttocks that feels like electricity that occurs with sitting and bending activities. She has incontinence and requires catherizations at times since her pain appears to worsen when she has a full bladder. She has persistent low back pain and feels like her pelvis is tearing apart at times in the region right buttock. There is numbness down the right lower extremity. It is difficult for her to wear tight pants since it causes pain in the region of her perineum. She has difficulty evacuating her bowels and she suffers with shooting pain into her anus. She has persistent numbness of her clitoris which decreases sensation during sexual activity. Her pain seems to improve when she sits on the toilet or lays on a recliner.
Medical perspective prior to the vaginal mesh debacle:
Pudendal neuralgia is a well described medical condition with a specific set of clinical symptoms that is often a slowly developing pain syndrome that potentially develops with or without known trauma, often misdiagnosed by uninformed medical providers who perform a variety of useless diagnostic tests, prescribe multiple medications, recommend a variety of ineffective invasive procedures, which all results in prolonged disability, declining function, and progressive depression.
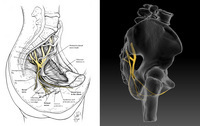
Pudendal neuralgia results from the compression or tension of the pudendal nerve anywhere along its course but appears most likely related to compression between the sacrotuberous and sacrospinalis ligaments. Other sites of compression include the piriformis muscle, and Alcock canal. Symptoms are directly related to the referred pain down the terminal branches that innervate the penis, the clitoris, and the anorectal area. Mechanisms of nerve damage include tension from chronic straining from constipation, squatting, and prolonged vaginal deliveries. Mechanisms of compression include prolonged bike riding or horse riding, and falls on the tailbone.
Historically pudendal neuralgia consists of symptoms affecting mainly the bowel and bladder dysfunction, sexual dysfunction, and anorectal pain. The primary researchers for the diagnosis and treatment of this disorder are from France and they described a set of diagnostic criteria (Nantes Criteria) for clinicians to refer to when evaluating patients with this disorder which include the following: ‘(i) pain in the anatomical territory of the pudendal nerve, (ii) pain worsened by sitting, (iii) the patient is not woken at night by the pain, (iv) no objective sensory loss on clinical examination, and (v) positive anesthetic pudendal nerve block’.
The most amazing component of this disorder is that the symptoms are clearly related to the compression of the pudendal nerve or the terminal branches of the pudendal nerve and despite this clear pattern of neurologic dysfunction that is referred from the pudendal nerve, the diagnosis is often missed. There are three branches to the pudendal nerve: 1) inferior rectal nerve that supplies the skin of the anus and the anal sphincter, 2) perineal nerve that supplies the vagina and the skin of the labia, 3) dorsal nerve of the clitoris (penis). Every symptom that the patient has is directly related to an impairment of the nerve or its terminal branches. Urinary symptoms include frequency, urgency, incontinence, and painful urination. Female sexual dysfunction includes pain on penetration, pain after sex, and decreased sensation. Bowel dysfunction is constipation, anal pain, inability to evacuate, and a feeling like there is an object in their rectum.
You may have a few questions:
Why was this diagnosis missed if it is so clearly related to a nerve distribution?
Simply said: it was very rare! (At least prior to the vaginal mesh debacle) In fact, to date I have never met a neurosurgeon or an orthopedic surgeon who has ever heard of this disorder. It is so rare that it is not taught during residency and until recently, has never been the focus of continued medical education. Complicating the issue are the untrained physicians who at times will miss the diagnosis; they will see a patient with these complaints, their symptoms are similar to other diagnoses and patients they have treated, so they merely perform the tests and the procedures that they commonly do, and then refer the patient away.
How did I diagnose my first patient?
Luck, maybe even fate. During my residency we were required to take a self assessment test to determine how we ranked compared to the other residents nationwide. I clearly remember there was one multiple choice question that asked the following question: What is the diagnosis of a person with incontinence, anorectal pain, and sexual dysfunction? Every answer from an anatomy standpoint didn’t make sense except pudendal neuralgia. Since I had never heard of this diagnosis I proceeded to the library and researched this disorder and it was clear that pudendal neuralgia had destroyed the lives of thousands of people and has received very little attention. This caught my attention then, and continues to be a major concern of mine today. To think about a person who suffers with sexual dysfunction, anorectal pain, and incontinence while their treating physicians have no reasonable diagnosis or treatment plan. The average time of onset of symptoms to diagnosis is seven years. The average number of doctors seen during this time is in double digits. The average number of unnecessary test and procedures are in the dozens. There have been suicides, the number unknown. Very sad, tragic.
Medical Perspective Post-Vaginal Mesh:
The history regarding the improper utilization of vaginal mesh is beyond the scope of this discussion. Clearly and undisputedly there are significant adverse medical events requiring ongoing medical care and repeat surgical procedures for complications such as mesh erosion, infections, incomplete voiding, painful sex, and pelvic pain. There is also indisputable evidence that this is a defective product that can cause pudendal neuralgia due to the traction of pudendal nerve or compression to the pudendal nerve. Treatment includes medications, physical therapy, diagnostic and therapeutic injections, and surgical decompression of the compressed nerve with removal of the mesh. There are two surgical techniques for decompression with approximately 60% improvement in pain and urinary and bowel incontinence. Each procedure has its unique complications and there is no consensus on which procedure is best. Hopefully with early diagnosis and effective treatment, the debilitating pain of pudendal neuralgia can be controlled. I also hope the publicity caused by the “vaginal mesh debacle” will help end its destructive path and help inform sufferers who continue to live in the dark, undiagnosed.
Live Care Planner Perspective:
What is a life care plan?
A patient of pudendal neuralgia will have significant and life-long medical and rehabilitation needs that may change as the patient ages. It is a life care planner’s role to provide a road map for the care of these patients to maximize function, reduce or eliminate complications, and improve the individual’s quality of life going forward. All recommendations must be medically necessary and must be appropriate. Patients with a pudendal neuralgia will benefit from a life care plan because it is a concise summary of current and future needs and their associated costs. It is essential evidence for court to prove damages related to injuries from a negligent act or a product liability case.
A life care plan is best devised by a medical profession who is a Certified Life Care Planner. The plan will likely be a multi-page document based on a clinical interview of the patient and family, review of the medical records, a psychological assessment, and communications with the treating physicians and other medical providers. Utilizing this information, the life care planner will follow specific methodologies based on published standards that are subject to peer review to devise a comprehensive plan.
A life care plan for a pudendal neuralgia patient will include the following: 1) Projected evaluations from medical professions such as physical therapy, 2) Projected therapies including physical therapy and psychological services, 3) Wheel chair needs and their accessories (if required), 4) Future educational needs and vocational assessment, 5) All future routine medical care including physician visits, medications, and medical supplies such as catheters, and 6) All future surgical care and hospitalizations. All needs will have a start date, frequency, stop date, and an associated cost.
Attorney Perspective:
Product liability law can favor injured parties against a party that manufactures, distributes, or sells a defective product that is the cause of the injured person’s harm. The injured party has to show that the product was defective in either design, by way of a manufacturing defect, or by inaccurate marketing of a product by way of failure to warn. So far there have been a few trials around the country that have found a mesh to be defective. On July 13, 2011, the Federal Drug Agency issues a warning to patients and the medical community that serious complications for vaginal repair for pelvic organ prolapse (POP) are not rare and there was no clear evidence that transvaginal POP repair was more effective than non-mesh repair. The FDA believed that the risk of complication is directly related to the mesh and not due to surgical error. Statistical analysis by the FDA revealed that pelvic pain occurred in 5.5-8.5 percent of patients and painful sex (dyspareunia) occurred in 1.6-7.3 of patients, and erosions occurred in 7.7-19% of patients. In essence the FDA has determined that pelvic pain is an unacceptable postoperative outcome caused by the vaginal mesh. With these findings there is definite evidence that patients should have been provided warning to adequately advise the risk of receiving the mesh.
Social Media Tags: pelvic pain, neuralgia, physical medicine and rehabilitation, misery, vaginal hysterectomy,






